Kaslyn Dao sat in the living room, playing with her rainbow-colored purse.
She grabbed another item on the mat.
“Mommy, what’s this?” she asked.
“Nail polish,” her mother, Natalie Nguyen, replied.
The 6-year-old then walked to the couch to enjoy one of her favorite animated TV shows, “Bluey.”

Her vision is gone, her gait is far from perfect, and her speech is limited, but Kaslyn’s condition on this day in early May 2023 has far exceeded the expected outcomes that a multidisciplinary team at CHOC ever imagined was possible.
Following a series of cardiac and neurological emergencies that began Jan. 7 and lasted more than two weeks, Kaslyn underwent high-risk surgery that doctors believed, in the best-case scenario, would leave her in an unaware and unresponsive state the rest of her life.
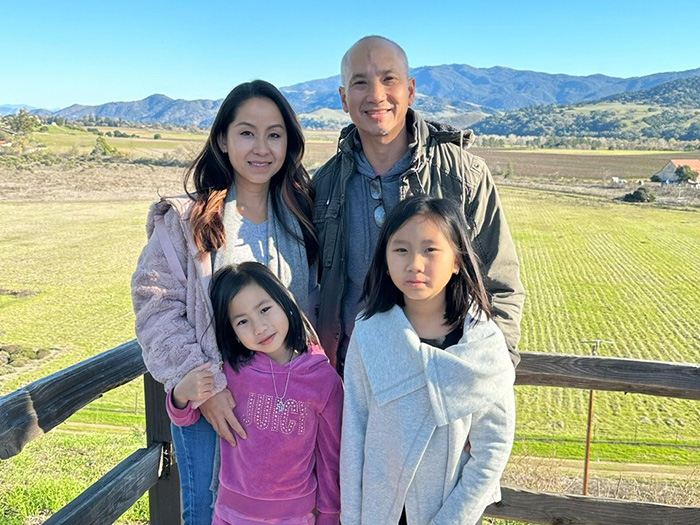
At the heart of her medical odyssey is a family – Natalie, her husband, Dean, and Kaslyn’s sister, Kara, 9 – who refused to give up on her.
“I knew I would take her home no matter her condition,” Natalie says. “And if God was going to make her an angel, I was at peace with that.”
Trial by fire
Kaslyn had her first fainting spell when she was 3 years old after she became agitated and cried.
Blood tests turned up nothing abnormal.
In late November 2021, when she was almost 5 years old, Kaslyn fainted while playing hide and seek.
Blood, heart, and brain tests again yielded no explanations.
Late on the evening of Jan. 7, 2023, Natalie sent Kaslyn to brush her teeth and prepare for bed – an ordinary night.
Kaslyn ended up on the bathroom floor unresponsive. An uncle rushed to her side and the family called 911 and performed CPR.
During transportation to a local hospital, Kaslyn suffered her first known cardiac arrest. The team called for help from CHOC.
Dr. Ancilla Rompala, a third-year critical care fellow at CHOC, went with a nurse and a respiratory therapist to pick Kaslyn up.
Dr. Jason Knight, medical director of the pediatric intensive care unit (PICU), was the attending physician.
The CHOC team arrived just in time as Kasyln’s clinical condition continue to deteriorate. Dr. Rompala quickly took charge of the situation and directed the team.
“That night felt like every simulation I had ever practiced as a physician all at once,” recalls Dr. Rompala, who found herself thrust into a leadership role that night.

Between rhythm stabilizing medications, electrical defibrillation (“shocking”), CPR, and replacing her breathing tube, Kasyln was briefly stabilized to allow a safe and quick transport to CHOC.
“It was a real team effort,” Dr. Rompala says. “Her heart rhythm was so abnormal that we couldn’t rely on the monitors. In fact, one nurse was instructed to keep a finger on her pulse at all times.”
Dr. Rompala says of those 90 minutes: “This would have been an intense situation for any physician. I remember telling myself I’m not going to let this kid die in this emergency room.”
A call at 3 a.m.
Kaslyn was taken to the cardiovascular intensive care unit (CVICU) where she went into cardiac arrest three more times.
Realizing the gravity of Kaslyn’s condition, Dr. Knight awoke thoracic surgeon Dr. Brian Palafox with a phone call at 3 a.m.
He was on call that morning for administering ECMO (extracorporeal membrane oxygenation), life-saving technology for children that takes over the heart’s pumping functions and the lung’s oxygen exchange.
Dr. Palafox, after Dr. Knight briefed him, knew ECMO was Kaslyn’s only chance.
Around 6 a.m. that morning, Kaslyn was placed on ECMO via cannulas that were inserted directly into her heart through the center of her chest.
“Think of a child getting ready to brush her teeth and a few hours later there’s a surgeon taking a saw to her sternum,” Dr. Knight says.
A prayer
The walls of Kaslyn’s home are lined with photos of her and her family enjoying a favorite pastime: hiking and touring Southern California.
In December 2022, Kaslyn and her family visited Mission Santa Barbara.
At the souvenir shop, Kaslyn picked out a crucifix necklace that she wore up to the moment the medical team had to remove it to perform the necessary steps to save her life.
Her mother now wears it.
During the ensuing medical ordeal, Natalie prayed.
“As a Catholic, I did everything to prepare her to go to heaven,” she recalls. “I prayed to Mary and told her, ‘Please don’t spoil her. Make sure she does her homework and take her on walks. Play with her.’”
Turn for the worse
After two days at CHOC that included whole genome sequencing, clinicians had a diagnosis: catecholaminergic polymorphic ventricular tachycardia (CPVT), a rare (1 in 10,000) heart rhythm disorder.
Caused by a gene mutation, CPVT is a too-fast heartbeat in the heart’s lower chambers triggered by high adrenaline levels, says Dr. Anthony McCanta, a cardiologist who specializes in electric issues of the heart. CPVT manifests itself by fainting and cardiac arrest.
After two days on ECMO, Kaslyn suffered complications including thrombosis, which revealed two major strokes in her brain. The CHOC team decided to take her off ECMO.
Fortunately, Kaslyn’s heart was able to function on its own without further arrythmias.
Then, two weeks later, her condition plummeted.
A tough choice
In his 20 years at CHOC, Dr. Knight has seen countless critical cases.
To some of Kaslyn’s physcians, her condition appeared hopeless.
“Each of these steps you’re thinking, ‘How’s she going to make it through all of this?’” Dr. Knight recalls.
On Monday. Jan. 23, after two weeks of stability and improvements, Kaslyn’s heart rate and blood pressure suddenly dropped overnight. An ultrasound revealed fluid around her heart and lungs
She was taken to the catheterization laboratory for yet another procedure: to place chest tubes to drain the fluid around her heart and lungs. Kaslyn again went into cardiac arrest.
Her kidneys and liver began to fail, causing bleeding everywhere: into her urine, from her mouth and nose, and into her brain. CT scans revealed the bleeding affected over half of the left side of her brain.
Four neurosurgeons – Dr. Joffre Olaya, Dr. William Loudon, Dr. Suresh Magee, and Dr. Michael Muhonen – discussed whether opening her skull to reduce brain swelling was worth the risk. Kaslyn’s thinned blood was a big concern. She could bleed out and die on the operating table.
If Kaslyn survived, the neurosurgeons agreed, she would possibly be neurologically devastated for life.
As much as the team wanted more than anything to save Kaslyn’s life, they knew the chances were slim, and that her family needed to know and understand the grim reality.
‘Please save my sister’
Pediatric critical care physician Dr. Andrea Guardenier was at bedside.
She believed the heavy medications Kaslyn was on were masking more signs of life then tests, including a pupillometry, which measures brain activity by reflecting light in the pupil of the eye, were indicating.
“She kept showing little glimpses of responses to pain and other changes which convinced me that surgery should be done,” Dr. Guardenier recalls. “Her mother, despite the tragedy of what was happening, was very realistic. She just wanted her daughter to live, and that was what she was fighting for – even if it was just a chance. That was important for Dr. Olaya and our entire team to hear.”

Dr. Diane Nugent, medical director of pediatric hematology, played a critical role at this time. She was able to reverse Kaslyn’s bleeding risk through a combination of treatments within two hours, setting her up for the best possible outcome.
Dr. Olaya didn’t expect to do much during the surgery: just remove a portion of her skull. The risk, he believed at the time, was too high to do anything more.
At some point, Natalie turned to Dr. Guardenier.
“What would you do?” she asked.
“I have seen children with this type of brain injury have incredible recoveries,” Dr. Guardenier replied. “We must give her a chance at life.”
Amid the serious discussion, Kaslyn’s sister, Kara, poked her head between the adults crammed into the room and addressed Dr. Olaya.
“Please save my sister,” she told him.
Dr. Olaya knelt down and looked into Kara’s eyes.
“I’m a dad, too,” he said. “I’ll try.”
Success with adecompressive craniectomy
Before surgery, Child Life specialist Lauren Schwarz took a fingerprint of Kaslyn for a necklace for her mother.
Kara visited her bedside to record songs as part of CHOC’s “memory making” service.
Natalie summoned a priest.
She whispered to Kaslyn just before she was wheeled off for surgery: “Any time you feel you don’t want to fight anymore, please let the nurses and doctors know and they will help you. You are always in mommy’s heart.”
Dr. Olaya, assisted by Dr. Louden, performed adecompressive craniectomy, a neurosurgical procedure in which part of the skull is removed to create room for her swollen brain room to expand.
Dr. Nugent had done a great job keeping Kaslyn’s blood appropriately thick. Dr. Olaya had time to go in and clean out blood and clots that were blocking blood flow and killing Kaslyn’s brain tissue.
He left a catheter in a ventricle of Kaslyn’s brain to monitor the pressure and closed the opening with skin.
After two hours, Dr. Olaya emerged from the operating room.
“Surgery was a success!” he declared.
No one, at the time, knew how much of a success it would turn out to be.
‘Thank you for saving my life’
Kaslyn remained in CHOC’s PICU until March 3, when she was sent to HealthBridge, a long-term pediatric care facility in Orange. There, she began physical, speech, and occupational therapy.
Dr. Guardenier saw her on March 3.
“She was sitting up, eating, and moving her limbs in a limited way,” Dr. Guardenier recalls. “She wasn’t speaking much – mostly just saying yes or no – but she was in great spirits.”
In late March, Kaslyn went home.
In mid-April, she and Natalie visited Dr. Olaya in his office.

“Thank you for saving my life,” Kaslyn told him.
On April 24, Dr. Olaya reattached the piece of Kaslyn’s skull.
“Coming back to CHOC for the skull re-attachment was like a homecoming,” Natalie says. “The team at CHOC is like family to us and we felt completely at peace in their hands.”
Over two days, doctors, nurses, therapists, and other team members involved in Kaslyn’s care came by to visit her.
“We were overcome with the love we received and gratitude we felt for the gift this amazing team here at CHOC had given us,” Natalie says. “Kaslyn’s progress has been called a miracle, but it would not have been realized without this exceptional team.”
‘Patients can surprise us’
The doctors involved in Kaslyn’s care say a well-orchestrated team effort saved her life – as well as a mother and family that came to terms with her condition and insisted that all steps be taken.
“Kaslyn’s a testament to everybody to never give up, to keep fighting hard,” Dr. Rompala says.
“We did everything at the highest level,” says Dr. McCanta, who will treat her from now on, “and if any one of those steps didn’t go well, she would have died.”
He adds: “I’m shocked at the neurological recovery she’s made.”
Kaslyn will remain on medications to prevent arrhythmias.
She will be able to go to school but likely will not be allowed to do sports, Dr. McCanta says.
“Kaslyn is a perfect example of the importance of not relying on scans alone, and that patients can surprise us,” Dr. Guardenier says. “She’s a perfect example of never underestimating the ability of a child’s brain to recover.”
Adds Dr. McCanta: “I’ve seen a lot of crazy stuff, but this is one of those cases that makes you cry. It is a testament to the faith of the family and the dedication of our entire team.”
Learn more about CHOC’s Neuroscience Institute.
Get more expert health advice delivered to your inbox monthly by subscribing to the KidsHealth newsletter here.

Learn more about CHOC’s Heart Institute
CHOC and UCLA Health together have been ranked among the top children’s hospitals in the nation for Cardiology & Heart Surgery by U.S. News & World Report.





