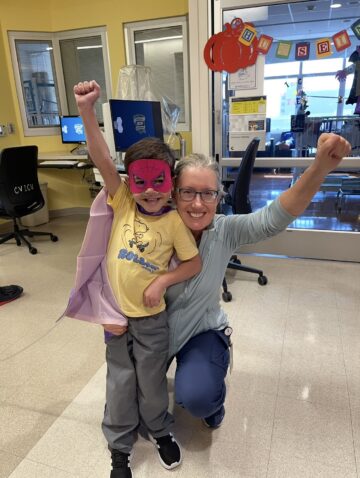
Five-year-old Emma has hypoplastic left heart syndrome (HLHS) and has undergone three open-heart surgeries since first coming to CHOC Hospital ― the only Orange County hospital providing pediatric open-heart surgery― at just 2 days old. After the last surgery, she went home with an advanced, wireless monitoring device provided by the CHOC Cardiopulmonary Health Intelligence Program (CHiP). This lightweight tablet monitors Emma’s blood pressure and other vital signs, instantly transmitting the data to her care team at CHOC who can incorporate it into her electronic medical record as needed. The tablet also offers her parents extra peace of mind and direct access to Emma’s team of specialists at CHOC.
Videoconferencing for “virtual visits” mean CHOC doctors, nurses and other members of her care team are always close by. It’s part of a larger pilot program that integrates several emerging health technologies to provide even more highly personalized care.
HLHS is a type of heart defect that occurs when the left side of the heart does not form properly during pregnancy. In patients with hypoplastic left heart syndrome, most of the structures on the left side of the heart are small and underdeveloped. The degree of underdevelopment differs from child to child. Perhaps the most critical defect in HLHS is the small, underdeveloped left ventricle. This chamber is normally very strong and muscular so it can pump blood to the body. When the chamber is small and poorly developed, it will not function effectively and can’t provide enough blood flow to meet the body’s needs. For this reason, an infant with HLHS will not live long without surgical intervention.

Babies born with this condition must begin the first of three open-heart surgical procedures within days of birth. Emma underwent her first surgery when she was 6 days old and had her third surgery almost four years later. After each surgery, her parents Patrice and Kevin saw noticeable improvement in her energy, mobility and quality of life.

But children like Emma need frequent office visits to monitor heart function, medication and symptoms. Over the past five years, her parents have made countless trips to CHOC, sometimes as often as every day. At home, they’ve meticulously tracked their daughter’s medications, blood pressure and overall health with pen and paper.
That changed last year thanks to a five-year CHOC pilot program designed to provide more personalized treatment for kids with heart failure. Emma’s parents now check her vital signs instantly at home with the same clinical accuracy as an office visit. With the Integrated Medical Tablet provided by the CHOC Cardiopulmonary Health Intelligence Program (CHiP), Emma’s doctors, nurses and care team are only a touch screen away.

“After her last open-heart surgery, Emma was still healing at home when we began testing out this machine,” Patrice said. “It gave us such peace of mind as we were still closely looking at her oxygen saturation and blood pressure. We didn’t have to go into the office every day to get this information—it could be recorded and sent to her specialists from the comfort of our own home.”
Instant Communication
Surgery may be behind her, but Emma continues taking medications that require constant monitoring and adjustment. The tablet has built-in alerts to notify her doctor if the results are outside the range of the personal limits that have been set for her.
And if something doesn’t look quite right, Patrice and Kevin don’t have to drive Emma over to CHOC. They can take photos and videos with the tablet and send them directly to Emma’s care team.

“Emma is on a diuretic for her heart condition, so being able to show her doctors if she is swollen or puffy is helpful,” Patrice said. “We are also able to type up our notes and questions for her doctors.”
Videoconferencing capabilities allow “virtual visits,” including wellness checks and parent education, at any time with the CHOC cardiopulmonary team. Beginning in 2018, CHiP will expand services to patients with other types of heart conditions.
“Patients and families feel much more comfortable outside of the clinical setting, but when they’re not in the hospital, they feel very nervous about the health of their child. They have much more peace of mind knowing that their child has quick access to CHOC from home,” explains Dr. Anthony Chang, CHOC’s Chief Intelligence and Innovation Officer, “We’re proud to offer a clinical environment to test and evaluate new technologies such as artificial intelligence and remote monitoring solutions.”

Far More Than a “Fancy Gadget”
Remote monitoring, video conferencing and wireless access to a patient’s electronic medical record are exciting advancements in care for children with heart failure. In this pilot study, however, CHOC is exploring the additional benefits that may come from leveraging these capabilities with other emerging health technology.
One of those technologies is precision medicine, a treatment approach that incorporates the patient’s genetics, environment and lifestyle. Another is pharmacogenomics, which evaluates how genetics may impact a patient’s individual response to a particular medication.
As a pediatric cardiologist within the CHOC Heart Institute, Dr. Chang is interested in how these technologies, combined with data analytics and artificial intelligence, may further personalize treatment and improve outcomes.
“Our goal is to use all available technologies and provide the most advanced, innovative care that is best suited for the individual patient,” Dr. Chang said. “CHOC is taking a national role among children’s hospitals to develop a model that may ultimately be used by other pediatric specialties for better management of complex patients.”
Get more expert health advice delivered to your inbox monthly by subscribing to the KidsHealth newsletter here.

Learn more about CHOC’s Heart Institute
CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2024-25 Best Children’s Hospitals rankings and ranked in the cardiology and heart surgery specialties.