What to do if your child has a fever
Fever is a common symptom in kids and can occur when a child’s body is responding to an infection, or as a result of an inflammatory process. A fever occurs when the body’s internal temperature rises above its normal level. Pediatricians usually consider a fever to be a temperature of 100.4°F or above (when taken rectally). A child’s body temperature will change naturally throughout the day. Although fevers are often a sign of a good response to an infection, knowing whether a fever requires medical attention can feel overwhelming for parents. In this guide, you’ll get all the information needed to decide how to best help your baby, infant or child when they have a fever.
Child temperature chart quick guide
| Child or infant’s age and method | Child or infant’s temperature | Where to take child or infant for care to treat fever |
|---|---|---|
| 1 month or younger (rectal) | 100.4°F (38°C) or higher |
|
| 1 – 3 months (rectal) | 100.4°F (38°C) or higher |
|
| 3 months or older (rectal, oral or underarm) | 102.2°F 102.3°F 102.4°F 102.5°F 102.6°F 102.7°F 102.8°F 102.9°F 103°F 103.1°F 103.2°F 103.3°F 103.4°F 103.5°F 103.6°F 103.7°F 103.8°F 103.9°F 104°F |
|
| 3 months or older (rectal, oral or underarm) | 105°F (40.5°C) or above |
|
Schedule a COVID-19 Test
If you think your child might have a fever from a COVID-19 infection, please schedule a testing appointment.

How to lower (break) a child’s fever
When a child’s fever is not emergent, the first goal should be to reduce the fever. Medicine, like acetaminophen or ibuprofen, is usually the fastest and most effective way to lower a kid’s fever. Infants and babies younger than 2 months old should not be given medicine for fever without a pediatrician’s visit.
How to reduce a child’s fever naturally
While medicine can be the most effective way to lower a fever, there are other methods that can be used alongside medication to help a child’s body fight their fever and keep them comfortable.
Food and drinks
Kids with fevers can lose fluids faster than usual and easily become dehydrated. Offer them plenty of fluids to avoid dehydration and avoid liquids with caffeine and high sugars, as these can worsen dehydration by causing urination and/or diarrhea. Appropriate drinks/foods include water, electrolyte beverages, soup, ice pops, and gelatin. Read our hydration guide for more info.
Rest
When a child has a fever, it’s best for them to stay home and get plenty of rest. While they don’t have to stay in bed all day, they should take it easy. Read our blog for sick day activity ideas.
Be cautious with sponging and baths
While sponging and bathing can help comfort a child with a fever, these methods are not recommended to treat a child’s fever. Baths only help cool a child while they’re in the water, but fevers may immediately return after they get out. If a bath helps comfort your child, be sure to use body temperature water. Anything cooler can lower their temperature too quickly. Couple this with medication to focus on eliminating the fever. Do not use alcohol baths at all.
Don’t bundle up
When a child has a fever, their higher internal temperature may make them feel cold or shiver. However, it’s important to make sure to not overdress or over-bundle a child, as this can prevent body heat from escaping — which is important to reduce their fever. Dress them in lightweight clothing and only use a light blanket or sheet in bed.
When to seek expert care for fevers in children
When to call a doctor for a fever?
Newborn: Under 1 month
- Has a rectal temperature of 100.4 °F (38°C) or above.
- Infants under 1 month should be taken to the emergency department right away.
Infant: Under 3 months
- Has a rectal temperature of 100.4 °F (38°C) or above.
- Infants 1-3 months with a temperature should be seen by a pediatrician. If your child cannot be seen by a pediatrician right away, visit your closest emergency department.
Child: Over 3 months
- Has a temperature between 102.2 °F (39°C) and 104 °F (40°C).
- Has a fever lower than 102.2 °F PLUS:
- Refuses fluids or is too ill to drink.
- Has lasting diarrhea or vomiting.
- Shows signs of dehydration.
- Complains of sore throat or earache.
- Your child has a separate chronic medical problem.
- Has a rash.
- Experiences pain when peeing.
Always call the doctor when:
- Fever lasts over 24 hours in children under 2 years old.
- Fever lasts over 72 hours in kids older than 2 years.
- Your child gets sicker despite their fever breaking.
- A fever doesn’t decrease (expect 1-2 degrees) after using fever-reducing medicine.
When should I take my child to urgent care for a fever?
Parents should take their child to urgent care for a fever when their symptoms require a call to the doctor (see ‘When should I call my child’s doctor for a fever?’ above) but you’re unable to reach a pediatrician or schedule an appointment. Infants under 3 months are the exception to this general guideline, as they should be seen in an emergency department if they can’t see a pediatrician.
If your baby under 3 months old has a rectal temperature of 100.4 °F (38°C) or above and you can’t reach their pediatrician, skip urgent care and head directly to the nearest emergency department.
When your child is experiencing a non-life-threatening fever, calling a pediatrician is always the best first step. Do not take a child to urgent care when they are experiencing life-threatening symptoms. Head directly to your nearest emergency department or call 911 (see ‘When should I take my child to the hospital emergency department for a fever?’ below).
When should I take my child to the emergency department for a fever?
Emergency departments are equipped for the most complex or critical needs. Fever requires a visit to the emergency department when:
- An infant less than 28 days old has a fever of 100.4 or more
- A child’s fever is at 105°F (40.5°C) and doesn’t decrease 1-2 degrees after taking fever-reducing medicine.
- A child’s fever is above 105°F (40.5°C).
Children should also be taken to the emergency department if they have a fever of any temperature and are also experiencing:
- Non-stop crying
- A bulging or sunken in soft spot (in infants)
- Extreme irritability or fussiness
- Sluggishness or trouble waking up
- A rash or purple bruise-like spots that didn’t exist before the sickness
- Blue lips, tongue or nails
- A stiff neck
- Severe headache
- Limpness
- Trouble breathing
- Seizures
- Moderate to severe belly pain

Tips to help assess the severity of a child’s fever
Fevers can occur as a response to a variety of conditions and do not always mean a child has a serious illness. It can feel challenging to know when to be concerned about your child’s fever. Below are some general tips to help guide you in deciding the severity of fever:
Accurate temperature
Make sure you take a child’s temperature accurately. Start by using a reliable digital thermometer and placing it in the right area (orally, rectally, or under the arm).
Age
Consider your child’s age along with their symptoms. If they are an infant 3 months or younger and have a rectal temperature of 100.4°F or higher, call your doctor or go to the emergency department immediately. If your child is between 3 months and 3 years old and has a fever of 102.2°F or higher, call your doctor. For older kids, take behavior and activity level into account. Watching their actions can help you decide if the illness is serious and should be checked out by a doctor.
Behavior
If your child is over 3 years old and they continue to play, eat and drink well, remain alert and smiling, have a normal skin color and their temperature comes down, their fever is likely no cause for concern.
How to take a child’s temperature accurately
Your child’s age determines how you should take their temperature. The best options include rectal (the most accurate), underarm or oral. Ear thermometers are not recommended.
- Infants from birth to 3 months old should have their temperature taken rectally with a digital rectal thermometer.
- Kids younger than 4 or 5 years old should have their temperature taken under the armpit, also known as axillary temperature.
- Children older than 4 or 5 years old can have their temperature taken orally, by holding the thermometer under their tongue.
Tips for taking an oral temperature
(for children older than 4 or 5):
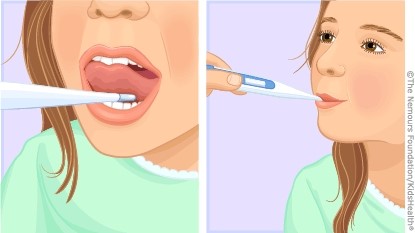
- Wait for 20 to 30 minutes after the child finishes eating or drinking
- Place the tip of the thermometer under the tongue toward the back and have them hold it with their lips
- Remind your child not to bite down or talk
- Wait until the thermometer beeps to remove
Tips for taking underarm temperature
(for children 3 months to 4 or 5 years):
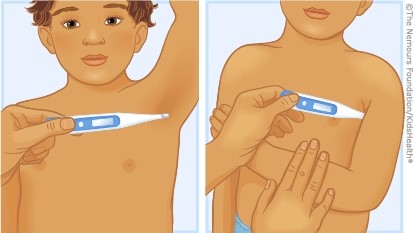
- Remove your child’s shirt and place a thermometer under the armpit (must be touching the skin)
- Fold the arm across the chest to hold the thermometer in place
- Wait until the thermometer beeps to remove
Tips for taking a rectal temperature
(for infants under 3 months):

- Wash the end of the thermometer with soap and cool water
- Apply a small amount of lubricant (petroleum jelly) to the end of the thermometer
- Insert the thermometer into the child’s anal opening about ½ inch to 1 inch, or until the tip is not visible
- Steady the thermometer between your second and third fingers while cupping your hand against your child’s bottom
- Wait until the thermometer beeps to remove
What is a fever?
A fever occurs when the body’s internal temperature rises above its normal level. Pediatricians agree that temperatures of 100.4°F or above (measured rectally) are considered fevers. Most children’s body temperatures change during the day, especially as they play. While a fever can be alarming, it usually causes no harm and can be a good sign that the body is able to fight infection.
Body temperature is controlled in the part of the brain called the hypothalamus. The hypothalamus knows the body temperature should be around 98.6°F and sends signals to the body to keep that temperature. When there is an infection, the hypothalamus will signal the body to raise the temperature. Most researchers believe this is done to create a less comfortable place for germs.
Fevers are classified based on how a child’s temperature is taken.
- 100°F when measured orally
- 100.4°F when measured rectally
- 99°F when measured under the arm
What causes a fever in children?
A fever is usually a sign or symptom of an illness or other underlying issue. While fevers can have many causes, there are a few common culprits:
- Infections: A fever is a sign that the body is responding to an infection or other process that causes inflammation. Common infections that cause fevers include bacterial and viral infections, such as flu, colds, earaches, strep throat, etc. Most fevers that result from the body fighting infections only last for a few days.
- Chronic diseases: When fevers last for more than a week or are recurring, they can be a sign of underlying diseases.
- Immunizations: After vaccinations like the flu shot, some kids will experience a low fever.

Common symptoms experienced during fevers
Besides having an elevated temperature, you can sometimes notice a fever through related visual symptoms like:
- Chills/shivering
- Body aches
- Headaches
- Sweating
- Hot skin
- Flushed appearance
- Fatigue/crankiness
- Loss of appetite
Call CHOC’s free 24/7 Nurse Advice Line
Our free nurse helpline is open 24/7 to address questions about your child’s health.
More information about fevers in children
The guidance on this page has been clinically reviewed by CHOC pediatric experts.
For more health and wellness resources from the pediatric experts at CHOC:
Sign up for the Kids Health newsletter.
The contents of this webpage, including text, graphics, audio files, and videos (“Materials”), are for your general information only. The Materials are not intended to substitute qualified professional or medical advice, diagnoses, or treatments. CHOC does not recommend or endorse any specific tests, physicians, products, procedures, or other information that may be mentioned on or linked to this webpage. Always call your physician or another qualified health provider if you have any questions or problems. If you think you may have a medical emergency, call your doctor, go to the nearest emergency department, or call 911.
For more health information for your family visit health.choc.org










