By Buffy O’Neil, mom of CHOC patient T.J.
When my youngest son T.J. was born, we were so excited to complete our family. His nursery was ready to go and we had picked out the outfit he’d wear home from the hospital. I’d even done genetic testing, and everything about T.J. looked fine.
I wanted to deliver my son at St. Joseph Hospital in Orange because I knew if anything happened, which I didn’t expect it to, CHOC was right next door. I drove all the way to St. Joseph when I was in labor so that we’d be close to CHOC if we needed them.
Even though T.J. was a bigger baby than we anticipated and I had a rough delivery, everything looked fine right after he was born. A minute later he started to turn blue. They thought it was because of the rough delivery. They gave him some oxygen, but he turned blue again. That’s when we knew something was wrong.
My delivery team paged a neonatologist from CHOC who rushed over to evaluate him. Within minutes, there was a neonatologist in our room, and then T.J. was on his way to the neonatal intensive care unit (NICU) at CHOC, and my husband went with him. That neonatologist suspected there was a problem with T.J.’s heart, and brought in two pediatric cardiologists, Dr. Fahrouch Berdjis and Dr. James Chu. Dr Chu performed an echocardiogram, also known as a cardiac ultrasound, and diagnosed T.J. with transposition of the great arteries. They reassured me that I hadn’t done anything wrong during my pregnancy that caused this. TGA is due to abnormal development of the fetal heart, which occurs during the first eight weeks of pregnancy.
The heart has four chambers and four valves. The problem in transposition of the great arteries is that the two main arteries leaving the heart come off the wrong pumping chamber. This makes the blood flow incorrectly and makes the baby sick at birth. In order for babies with TGA to have a chance at survival, they need a diagnosis within hours of birth, and then an immediate procedure called a balloon artrial septostomy. During this procedure, a special catheter with a balloon in the tip is used to create an opening in the wall between the left and right atria, to improve the mixing of oxygen-rich and oxygen-poor blood.
On the first day of T.J.’s life, nothing happened as we had planned, but everything happened as it should. I can’t even imagine what it would’ve been like if something had gone wrong. I thank God every day that T.J. was born at St. Joseph Hospital and CHOC was right next door. The doctors told us that many babies that have to be transferred to a children’s hospital to be evaluated have died in the process. Because T.J. was born at a facility that’s literally connected to CHOC (via an underground tunnel), he was able to be diagnosed and had his procedure done within hours.
The first week of T.J.’s life was really scary. His right lung collapsed and then got a little stronger, only to have his left lung collapse. Babies with TGA need to have their first open heart surgery in the first week of life, and we weren’t sure if he was even going to live long enough to have that surgery. Doctors, nurses and respiratory therapists did everything they could to stabilize him.
Everything was very overwhelming. The baby who we had expected to be perfectly healthy was lying in a hospital crib with a lot of wires and monitors attached to him. He was so close to dying. All we could do was sit, watch and pray he would survive.
Every doctor we met with was so patient and explained everything in a way we could understand. We were overwhelmed and just trying to take it all in.
After a scary six days, T.J. was stable enough to undergo his first open heart surgery called an arterial switch. During that procedure, Dr. Richard Gates pediatric cardiothoracic surgeon and co-medical director of CHOC’s Heart Institute, cut open T.J.’s chest, cut his arteries and switched them so they were in the correct spot, and then stitched them into place.
Five hours after we kissed our son goodbye and saw him being wheeled back into the operating room, Dr. Gates came out to meet us in the waiting room. He said the surgery had been difficult but overall it went well, and now everything was all up to baby T.J.
In the week after T.J.’s open-heart surgery, he wasn’t breathing as well as we hoped he would. His team decided to do a cardiac catheterization procedure to determine why he still had a murmur and issues with his oxygen levels. During that procedure, they placed a wire, mesh device called a stent in a narrowed artery to keep it open and improve blood flow.
After this, T.J.’s oxygen levels improved, but his heart and lungs had been through a lot and needed to grow stronger before we could go home. Our next big hurdle was getting T.J. to eat on his own. Our feeding specialist was surprised at how fast he caught on to sucking and swallowing, but because his body was working so hard to recover from surgery, he was burning more calories than he was taking in. The doctors decided it was best to place a percutaneous endoscopic gastronomy tube (more commonly known as a G-tube or feeding tube) directly into T.J.’s stomach so he wouldn’t have to work so hard to eat, but he’d still get the calories he needed to grow stronger.
Another unexpected hurdle was when T.J. started having withdrawals from the pain medication he had been placed on after surgery. A registered nurse/pain specialist was assigned to us in order to evaluate how best to help T.J. cope. She put him on a 30-day weaning plan and after a few days he started improving, and soon we were on our way home!
We were so happy to finally take our baby home, almost six weeks after he was born. We went home with a lot more than we came with, including a medication schedule with six different drugs outlined by his nurses, plus a breathing machine.
We knew T.J. would need another open-heart surgery before his first birthday. We had periodic appointments with his cardiologist Dr. Chu, and a feeding specialist as well. A few months later, Dr. Chu performed a cardiac ultrasound or echocardiogram to see how T.J.’s heart was working. He told us that even though T.J. had grown a lot and was healthy, it was time for his surgery. His arteries were not growing enough to keep up with him.

T.J.’s second open heart surgery occurred when he was six months old, and he had a third surgery when he was 18 months. Each of those were to expand arteries to allow for better blood flow. As a parent, I always appreciated Dr. Gates’ honesty. He told us that these were intense surgeries, and that T.J. would need blood transfusions during them to compensate for blood loss during surgery.
After the second and third surgery, we spent a week in the cardiovascular intensive care unit (CVICU) at CHOC. We were blown away at how the nursing staff cared for our entire family during that time. We were putting our son in their hands, but they didn’t just take care of him. They took care of all of us. Years later, the nurses that cared for him when he was a baby still want to hear updates about T.J. and how he’s doing in school.
For the first 18 months of T.J.’s life, it felt like we were at CHOC all the time. It was an unexpected start to my son’s life, and at the time, it was devastating. I felt like I was the only mom experiencing this, and if there’s any moms reading this I want you to know that you’re not alone. There are people out there who understand what you’re going through. Ask your child’s care team if they can put you in touch with other families who may be willing to share their stories with you. For my husband and me, being able to meet people with the same conditions, and to share stories with other adults who have been through what you’ve been through was incredibly helpful.
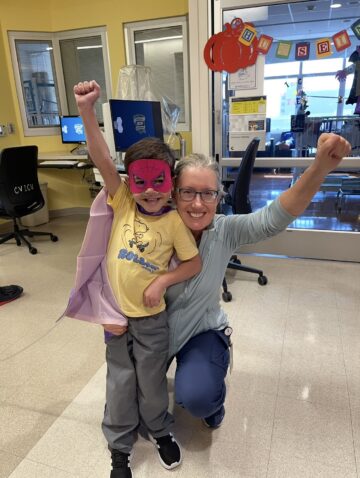
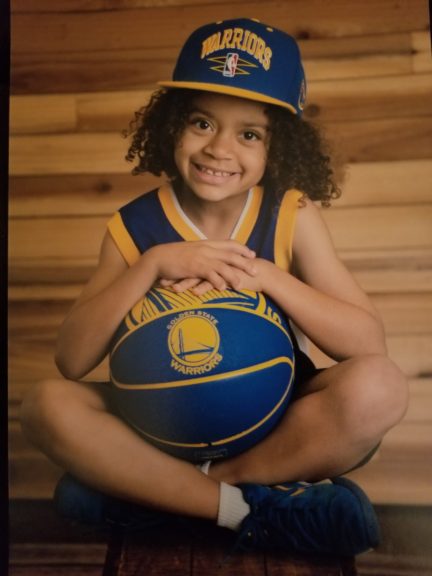
Today, T.J. is a happy eight-year-old. He’s very athletic and loves to play sports, and I’m proud to say he is a straight-A student. When he feels self-conscious about his scars, we remind him how special and strong he is. Even though his life has been filled with several surgeries and countless doctor’s appointments, he has no anxiety about going to the doctor’s office because he’s always treated so well there. When T.J. was a baby we saw Dr. Chu monthly, and now that his heart is doing so well, we only have to go twice per year.
As for my heart, I have a very special place in it for CHOC― especially for Dr. Gates and Dr. Chu. Both of them are in photos in T.J.’s room. We remind them at every appointment that they are the reason T.J. is alive.
Get more expert health advice delivered to your inbox monthly by subscribing to the KidsHealth newsletter here.

Learn more about CHOC’s Heart Institute
CHOC and UCLA Health together have been ranked among the top children’s hospitals in the nation for Cardiology & Heart Surgery by U.S. News & World Report.