CHOC and UCLA Health teamed up to save a patient with heterotaxy, a rare congenital heart defect
The mother, racing to the hospital, asked the clinician on the phone if her daughter Olivia was still alive.
“Not at the moment,” the clinician said.
The words floored Tamika LeBlanc, who fought to keep her composure as she and her husband, Willie, continued on their way to be with their 2 ½-year-old daughter, Olivia, as she embarked on the biggest fight of her life.
Sick hearts sometimes stop working well, for reasons that are not always well understood. Olivia’s unique heart was too weak to work on its own.
Born with severe CHD (congenital heart disease) and having persevered through several surgical interventions, Olivia crashed and was critically ill on a heart-lung machine as she waited for a new heart from a donor.
Heart transplant programs are built to expand therapy, infuse hope, and to make miracles possible.
And so began the miracle of Olivia.

A fruitful CHOC-UCLA Health collaboration
Olivia’s journey highlights the collaboration between CHOC and UCLA Health that began several years ago and was formalized in July 2023, with the primary goal of elevating pediatric cardiac care.
The collaboration, created to enhance access to world-class pediatric congenital cardiac care for children and their families across Southern California, is led by internationally recognized pediatric heart surgeon Dr. Glen Van Arsdell, who cares for children at CHOC and at UCLA Mattel Children’s Hospitals.
Olivia was born with heterotaxy (“different arrangement”) syndrome, a rare birth defect that affects the formation of the heart and other organs.
Pediatric cardiologist Dr. Nita Doshi of the CHOC Heart Institute diagnosed the complex heart defect in utero when Tamika was 21-weeks pregnant. The diagnosis is associated with an overall poor survival.
“Dr. Doshi told us it would be a long road,” Tamika recalls, “but she gave us a lot of hope.”
That hope would be remarkably tested after birth.
Heterotaxy, a rare congenital heart defect
Olivia’s heart had a single functioning pumping chamber “ventricle” – instead of two – and the blood vessels returning blood from her lungs to her heart had a narrowed path. This caused her blood oxygen saturation levels to be low.
After Olivia was born, Dr. Gira Morchi, chief of cardiology at CHOC, helped stabilize her. Dr. Morchi’s colleague, Dr. Michael Recto, performed heart catheter insertions.
To palliate the rare defect, doctors – typically in a minimum of three surgeries from when a newborn is just weeks old to when they’re between 4 and 5 years old – reconstruct the veins that carry “blue” (oxygen-poor) blood directly to the lungs without passing the heart. The “red” (oxygen-rich) blood then returns to the heart from the lungs and flows to the organs in the body.

Olivia had her first open-heart surgery when she was 18 days old and her second when she was 5 months old. She suffered a stroke when she was almost 2 years old, and things then took a turn for the worse a couple of months later when she experienced an abnormal heart rhythm that caused her heart to become sicker.
CHOC doctors, including Dr. Doshi, believed Olivia had not grown enough for the third surgery and given how sick her heart had become, likely wouldn’t survive. The CHOC and UCLA cardiac teams urgently reviewed her case and recommended a heart transplant.
A mother’s determination
In mid-December 2019, while at UCLA Mattel Children’s awaiting a heart transplant, Olivia, almost 2½ years old at the time, “coded” – her heart failed.
As her parents raced up the freeway, urgent life-saving measures began as she went into cardiac arrest. One of Tamika’s sisters, Shaun, who often relieved Tamika and Willie, was with Olivia at the time. She called Olivia’s parents to tell them they needed to come to the hospital immediately.
Nurses and doctors began chest compressions to pump blood in place of Olivia’s failed heart.
Simultaneously, surgeons began operating to put her on a life-saving machine for the sickest of patients called ECMO, which takes over the heart’s pumping functions and the lung’s oxygen and carbon dioxide exchange.
Tamika and Willie finally arrived.
As clinicians continued chest compressions on Olivia, and the surgeons operated, Tamika stood outside the room and refused to leave.
“She kept repeating, ‘My daughter will not leave here in a box,’” says Dr. Reshma Biniwale of UCLA Health. “She was determined that Olivia would live, and I think that determination impacted the surgical team.”
After 45 minutes of chest compressions, Olivia – a true heart warrior – did not give up.
‘Unusual’ procedure
A substantial percentage of patients put on ECMO for a prolonged period don’t survive, and being on it a week is considered a long time.
“One of our concerns is she had a head bleed in the past so we were very concerned about her overall status as well as her kidney function,” recalls Dr. Biniwale, who at Dr. Van Arsdell’s instructions inserted a cannula directly into Olivia’s heart. The tube typically is inserted into a vessel from the neck that connects to the heart.
“It was an unusual thing that we had Dr. Biniwale do,” recalls Dr. Van Arsdell. “This procedure was modified specifically for Olivia, and we didn’t know if it would work.”
Fortunately, over the course of wrenching days and weeks, Olivia responded nicely and was cleared for the heart transplant while she remained on ECMO. At this point, she had been on ECMO for nearly six weeks.
“It was profound that she was able to survive on the ECMO circuit for that long without succumbing to the complications,” Dr. Doshi says.
Extremely high-risk heart transplant
Usually patients who undergo a heart transplant while on ECMO face an extremely high risk of not surviving, Dr. Biniwale says.
“There’s a lot of bleeding because they’ve been on blood thinners and their blood has been churning through tubes for a long time without the ability to clot,” she explains. “Plus, having to go back into Olivia’s chest again after her prior surgeries also posed a risk.”
Olivia received a new heart in a transplant performed by Drs. Van Arsdell and Dr. Biniwale, who led the 12-hour surgery on Jan. 26, 2020.

The heart came from a 3 ½-year-old girl.
“Dr. Van Arsdell was instrumental in guiding me on what repairs needed to be done on her heart itself, on the old vasculature, before we put in the new heart,” Dr. Biniwale recalls. “Between the two of us, Olivia had a very good outcome.”
A heart transplant is not a cure.
“It’s exchanging one heart condition for a different, equally involved heart condition,” Dr. Doshi explains.
Olivia, who turns 7 this August, will require lifelong monitoring. She remains in therapy for delayed speech.
Heart families need support
Olivia’s relatives, including Shaun and two of Willie’s cousins, Leslie and La’Ron, were instrumental in getting her parents through their draining medical journey.
“Whenever they called, we were there to do whatever they needed,” La’Ron says.

Says Tamika: “We’re so blessed to have the tribe that we have.”
“I know the stress was a lot for them,” adds Shuan. “Heart families need to know how important being supportive is to the loved ones going through this.”
Dr. Morchi says Olivia’s story is a great example of how the CHOC-UCLA Health cardiac care collaboration is working.
“This is what we’ve been working on for years,” Dr. Morchi says. “We’re two institutions with different but significant strengths that can play off each other’s areas of expertise.”
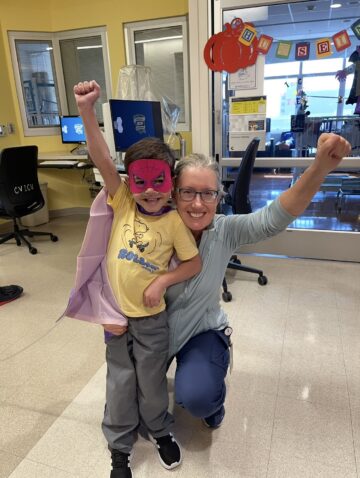
The superstar
Dr. Morchi, along with Drs. Doshi and Van Arsdell and Biniwale, attended last summer’s CHOC Heart Reunion at the Santa Ana Zoo.
Dr. Van Arsdell walked up to Olivia and crouched down beside her to pose for a picture.
“Is this the superstar?” Dr. Van Arsdell asked her.
Tamika and Willie started crying.
“We’re beyond thankful for CHOC and UCLA for the outstanding care Olivia received,” Tamika says.
Dr. Arsdell and other clinicians praised Olivia and her family for being critical to helping her achieve a remarkable outcome.


“It was one of those cases that was against the odds,” says Dr. Van Arsdell, chief of congenital cardiovascular surgery at UCLA Health. “As care providers, sometimes we’re amazed at the resilience of our patients, and Olivia is one of those patients.”
Today, Olivia is an energetic first-grader who loves playing in parks, ballet class, the color pink, eating, striking yoga poses in front of mirrors, and playing games on her tablet.
Tamika continues to support other heart families and has created OG LIFE, a website of resources to support heart families.
“There were people praying for Olivia all over the world,” Tamika says. “I still have people reaching out sharing with me how witnessing her story unfold has renewed their own faith and in some cases, has made them believe in miracles.
“As for me, I never doubted that my child wouldn’t make it. It wasn’t an option.”
Get more expert health advice delivered to your inbox monthly by subscribing to the KidsHealth newsletter here.

Learn more about CHOC’s Heart Institute
CHOC and UCLA Health together have been ranked among the top children’s hospitals in the nation for Cardiology & Heart Surgery by U.S. News & World Report.