“Compassion is CHOC’s middle name,” says Emily Fusco, mom of 13-year-old CHOC patient Henry, as she reflects on the compassion, kindness and expertise shown by CHOC’s doctors, nurses, child life specialists and support staff during Henry’s two-week stay at CHOC Hospital in Orange.
It all started on Feb. 7, 2022, when Emily received a phone call that every parent dreads. It was Henry’s school, stating that there had been an emergency. Emily rushed over to find Henry unconscious and in the care of paramedics. She learned that at lunchtime, Henry was outside getting ready for a game of football when he collapsed, started shaking and was not responding. He had gone into pediatric cardiac arrest and stopped breathing.
The paramedics arrived and found Henry to be in ventricular fibrillation — an extremely fast, abnormal heart rhythm that when left untreated can lead to sudden cardiac death. Fortunately, the paramedics successfully defibrillated Henry using an automated external defibrillator (AED), and then resuscitated and stabilized him.
With no prior heart issues, Emily was shocked and scared for Henry’s life. He was taken to the nearest hospital but was quickly transferred to CHOC Hospital in Orange to receive the pediatric-focused care that he needed.
The importance of CHOC’s pediatric-focused care
On the ride over in an ambulance bearing the image of Choco, CHOC’s beloved mascot, the CHOC’s transport team gave Emily comfort. She knew they were on their way to where Henry was supposed to be.
Henry spent the next two days unconscious and ventilated in CHOC’s Josie Y.S. Lee Pediatric Intensive Care Unit (PICU). Emily was so grateful for the CHOC staff during this time. “Everyone we encountered did their best to comfort us during the challenging and scary time of waiting for Henry to wake up, and not knowing how he would be when he woke up,” says Emily.
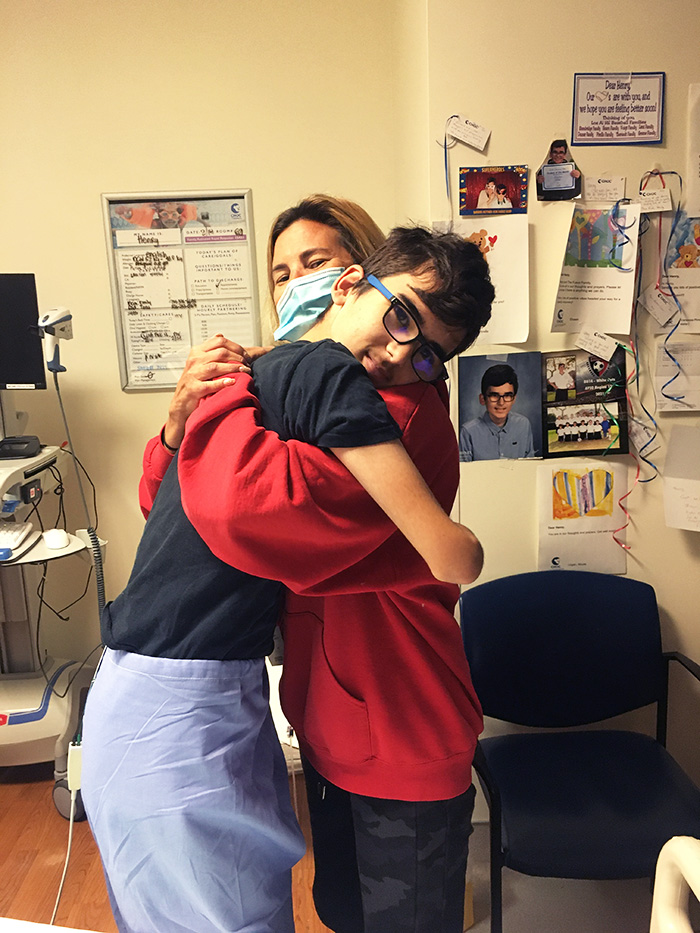
Fortunately, Henry soon woke up, looked around and easily recognized his dad who was in the room with him. Over the next few days, he was able to slowly wean off his ventilator.
While in the PICU, Henry then underwent a series of tests including an electrocardiogram (ECG); an echocardiogram or ultrasound of the heart; an electroencephalogram (EEG), which evaluates for seizures and brain activity; an MRI of the heart and the brain; and genetic testing to evaluate for any genetic cause of his cardiac arrest. CHOC doctors from multiple specialties teamed up to determine what may have caused this, and CHOC’s physical therapy (PT) and occupational therapy (OT) teams assisted in his physical and intellectual recovery.
Heart arrhythmias and implantable cardioverter defibrillators (ICDs)
All of the tests ran in the PICU returned with reassuring results that Henry had normal cardiac structure and function, and there was no electrical predisposition to arrhythmias or identifiable genetic cause that led to his cardiac arrest.
Dr. Anthony McCanta, a pediatric cardiologist specializing in electrophysiology at the CHOC Heart Institute, determined that the cause for Henry’s sudden cardiac arrest was idiopathic ventricular fibrillation, which means that it has no identifiable cause for his irregular heart rhythm. Henry’s family will be undergoing further genetic testing.

Super Bowl LVI.
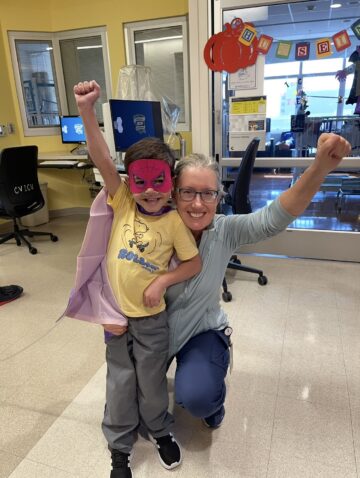
To prevent this from happening in the future, Dr. McCanta performed a procedure to implant an implantable cardioverter defibrillator (ICD) under Henry’s skin. An ICD is a small, electronic device that connects to the inside of Henry’s heart, detects potentially life-threatening arrhythmias and sends a life-saving pulse to the heart to convert the abnormal rhythm to normal. Henry’s ICD will constantly monitor his heart and provide a shock if it is ever again needed.
Just one day after Henry’s ICD was implanted, he was able to go home.
Now, Henry is able to attend school at home, eat full meals, play video games, practice his physical therapy exercises and go on walks. Although he can’t yet run or play his favorite sports soccer and football, he’s improving daily. Henry is looking forward to returning to school part-time in the coming months, and ultimately, he should be able to resume sports and other athletic activities. Henry will continue to visit CHOC for follow-up appointments with Dr. McCanta.

Advice for other families with kids who have gone through cardiac arrest
Emily says, “It’s so neat to see Henry progressing. He’s stronger than I ever thought he was and taught me that I am also stronger than I thought I was.”
To other families that may go through a similar experience, Emily explains that she leaned on her faith, and accepted help from family and friends. She advises families to try to stay positive, but also stay aware. She never expected that her 13-year-old could go into cardiac arrest, and advises parents to be aware of the symptoms of cardiac arrest and get genetically tested, if possible.
“It is so valuable to get all the information about what happened and why,” says Emily.
Warning signs and symptoms of cardiac arrest
The symptoms of cardiac arrest can be immediate and drastic — much like Henry’s symptoms. Someone experiencing cardiac arrest may:
- Suddenly collapse.
- Have no pulse.
- Not be breathing.
- Experience a loss of consciousness.
If your child is experiencing any of the symptoms of cardiac arrest. Call 911 or seek immediate medical attention.
Sometimes, you may be able to look for warning signs that someone is going into cardiac arrest. These signs include:
- Chest pain or discomfort.
- Shortness of breath.
- Weakness in the body.
- An increased heart rate, fluttering or heart palpitations (heart pounding).
But sudden cardiac arrest often occurs with no warning.
Make sure your child’s school or gym has an automated external defibrillator (AED) that can save the life of someone experiencing cardiac arrest.
Learn how to prevent sudden cardiac arrest in children.
Get more expert health advice delivered to your inbox monthly by subscribing to the KidsHealth newsletter here.

Learn more about CHOC’s Heart Institute
CHOC and UCLA Health together have been ranked among the top children’s hospitals in the nation for Cardiology & Heart Surgery by U.S. News & World Report.