Responsive neurostimulation (RNS) can help permanently treat seizures in select candidates
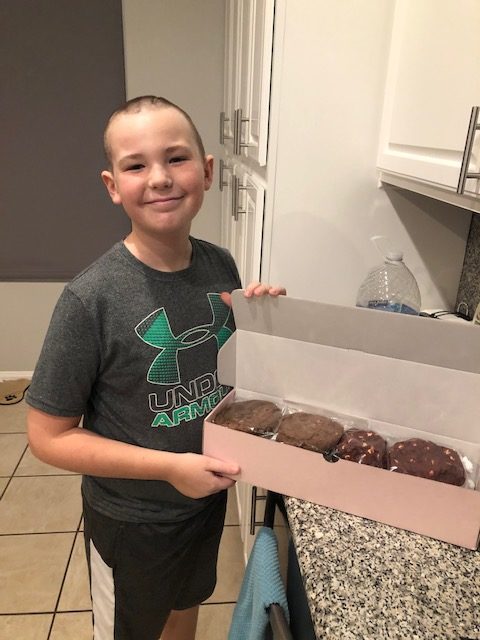
Bryce, age 11, is a thriving, active and intelligent pre-teen that loves to play sports and video games.
But when he was just 3 years old, he had a brain tumor growing near his motor cortex — the area of the brain involved in the planning, control and execution of voluntary movements. For treatment, Bryce had undergone a complete tumor resection via craniotomy, which is the surgical removal of part of the bone from the skull to expose the brain for surgery.
Unfortunately, by the time he turned 5 years old, Bryce started to experience breakthrough seizures, indicating that his tumor was growing back.
Unexpected seizures
During these breakthrough seizures, Bryce’s right arm would go completely numb for 30 seconds, and he would not be able to move it for about a minute after. Occasionally, the numbing sensation would even move down to his leg or affect his face.
“Nothing seemed to spark them,” says Jennifer, Bryce’s mom. “These seizures could happen any time, with no rhyme or reason of when or how often.” They often interrupted Bryce’s active lifestyle.
To combat the seizures, Bryce had tried all different kinds of medications. Jennifer says, “The side effects were becoming intolerable. I just didn’t like putting more and more drugs into his body,”
RNS treatment at CHOC
Looking for a more permanent solution, Bryce and Jennifer met with Dr. Donald Phillips, CHOC neurologist, regarding a therapy called responsive neurostimulation (RNS) to treat epilepsy. RNS involves having a small neurostimulator, similar to a pacemaker, implanted within the skull connecting two wires that are placed on the surface of the brain, in the brain, or a mixture of both.

Once implemented, the neurostimulator monitors and responds to brain waves to detect seizure activity. When this activity is detected, the stimulator sends a signal of electrical current to the brain to stop the seizure or possibly prevent the seizure. The RNS System wirelessly collects information from the neurostimulator and uploads it to a database where a provider can review a patient’s seizure activity and progress.
While RNS is currently only FDA approved for patients 18 years and older, CHOC can offer this to select patients that meet a certain criterion. Typically, the candidates for this system have multiple areas of seizures or have seizures coming from an eloquent area — the area on the surface of the brain necessary for language, motor and sensory functions — like Bryce’s tumor near his motor cortex.
Surgery offers seizure control
Jennifer was thankful for the opportunity that Bryce could receive this treatment at age 10 rather than having to wait until he was 18. She knew Bryce’s tumor regrowth would have to be treated eventually, and RNS allowed the opportunity to permanently treat the tumor and seizures at once — while he was young and resilient.
A year ago, Bryce had his RNS surgery at CHOC Hospital in Orange. During the surgery, partial resection of the tumor was performed and RNS wires were placed over the part of Bryce’s brain where his seizures usually occurred, protecting the area that controlled his hand function. Bryce stayed at CHOC for three days for monitoring following his surgery, then recovered quickly at home with no complications.
Nearly seizure-free
The responsive nature of the RNS System detects abnormal seizure activity and reacts in real time. With his, Dr. Phillips can track Bryce’s seizures as they occur, making changes to the RNS device over time for even better seizure control. Now, one-year post surgery, Bryce is nearly seizure-free.
“I occasionally have a bit of tingling in my fingertips, but it doesn’t stop me from playing basketball,” he says.
Jennifer quickly adds, “He is doing really well in school.”
Dr. Phillips is delighted that Bryce is now nearly seizure-free, now one year post his RNS treatment. CHOC aims to expand access to the RNS treatment for the pediatric epilepsy population through participation in a multicenter clinical study. This treatment shows exciting promise to help more pediatric patients like Bryce.
Get more expert health advice delivered to your inbox monthly by subscribing to the KidsHealth newsletter here.

Learn more about CHOC’s Neuroscience Institute
CHOC Hospital was named one of the nation’s best children’s hospitals by U.S. News & World Report in its 2025-26 Best Children’s Hospitals rankings and ranked in the neurology and neuroscience specialties.





