Just like some people take medications for other medical conditions like Asthma or Diabetes, some people also benefit from medications for things like depressed moods or anxiety. Medications can help lessen or control symptoms to help children get back to normal activities like before their symptoms started. A lot of times, doctors will use medications combined with individual or family “talk” therapy, as the medications can help the child feel comfortable enough to engage in therapy to learn skills to manage the feelings.
What do the medications do?
We know that there are certain changes in the brain that are related to many mental health illnesses. There are medicines that can help fix those changes. The most commonly used medications are anti-depressants, which are sometimes referred to as “SSRIs”. These medicines work on specific ways the brain sends messages. For example, SSRIs work on something called serotonin. In depression, serotonin levels appear to be low, so these medications help raise serotonin up to higher, healthier levels. It takes a while for the brain to get back to using this new level. So there is usually a delay from when people start medications to when they start feeling better. That’s also why your doctor will likely recommend your child continue taking the medications even when they’re feeling better, as the brain may need some more time to get back to normal.
Will my child become addicted or dependent on mediation?
Many parents worry about whether medications could lead their child to become addicted. Generally, medications that have a potential for addiction or dependency tend to be ones where there is a strong, immediate response. People become addicted because it makes them feel so good so fast. As you just learned, anti-depressants are not one of these medicines. This is a classic example of when slow and steady wins the race.
Medications (like SSRIs) are started at lower amounts and then increased slowly to help limit side effects and make sure your child isn’t getting more medication than they need. An increase in the dose doesn’t mean that your child is becoming addicted to the medication, it just means that they weren’t on a high enough dose yet, or what we call a “therapeutic dose”.
In some cases, your child’s doctor may suggest different medications to help your child’s symptoms. Some of these medications may have a potential for addiction but when used short-term and with proper supervision, they can be still be used safely. Your doctor will review all of this with you before starting any medicine, but be sure to ask any questions you may have.The good news is, there is the potential to eventually come off of the medication. Talk to your doctor about when that time might be for your child so that they can work with you to make sure it’s done safely (under the supervision of a professional and at the right time).
What about all the talk about medication making children suicidal?
You may hear that in some studies, some teens that were taking anti-depressants had more suicidal thoughts than teens who were not on anti-depressants. However, what we’ve found out over the years is that not treating depression can be even more dangerous. What this means is, if the doctor feels that your child’s depression is severe enough to require medications, they are likely already at high risk for suicidal thoughts. If they do come up, your child’s doctor will work with you to make the best plan to manage these thoughts.
What should I expect?
For the first two weeks of treatment, the main thing to watch for is side effects. Common side effects include stomach upset, nausea, headache, dizziness, change in appetite or sleepiness. Some side effects get better within the first week or so but may come back again for a short period of time if the amount of medicine is increased. If the medication makes your child dizzy or sleepy, generally we will recommend having them take it at bedtime.
Improvements tend to start gradually after a couple weeks. Sometimes parents will notice changes before the child is able to identify that they feel better. They may talk to the family more or get less upset about things. There will still be times that your child gets anxious (ex: big tests) but the anxiety may be less than it was before. Or even though they’re anxious they may be able to work through the anxiety better. If it’s been over a month and they’re not getting any better, it may mean that your child needs more medicine or needs a different medicine. Talk to your child’s doctor so they can help you figure out what will best help your child feel better.
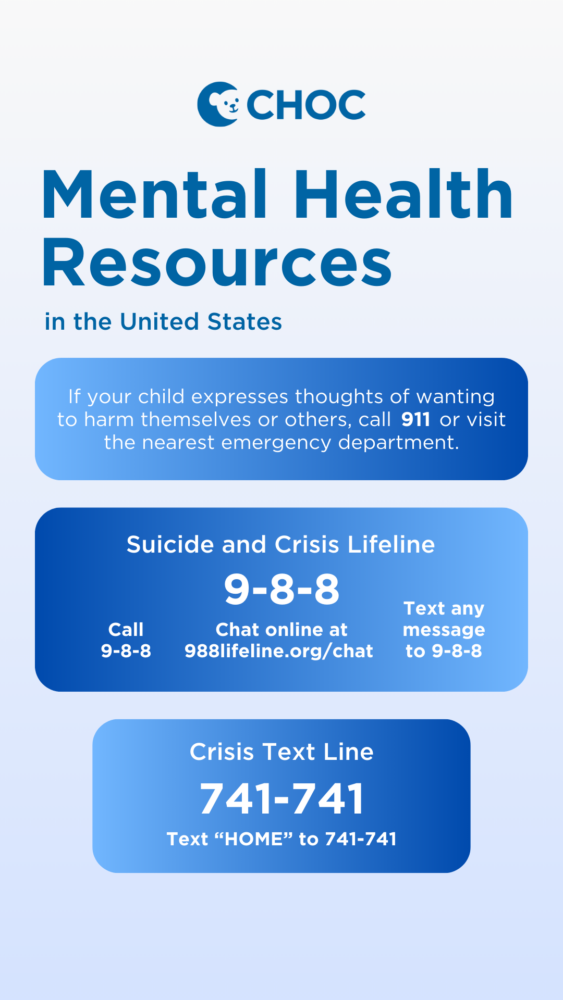
Crisis Resources
If your child expresses thoughts of wanting to harm themselves or others, call 9-1-1 or visit the nearest emergency department.
988 Suicide and Crisis Lifeline:
Call 9-8-8
Text any message to 9-8-8
Chat online at 988lifeline.org/chat
Crisis Text Line:
Text “HOME” to 741741
Save for later
Download, print or share on social media.
Learn more about CHOC’s pediatric mental health services
At CHOC, we specialize in providing a full spectrum of pediatric mental healthcare, including inpatient, intensive outpatient and outpatient program services.